When Fred Moore, 58, visited a CenterWell Senior Primary Care clinic in Las Vegas, he was suffering from debilitating health conditions: neuropathy in his feet and legs, shoulder pain, an inguinal hernia, asthma, allergies, and other upper respiratory issues, including bronchitis. Unable to work, he and his dog, Batman, were unhoused.
Moore selected CenterWell—a Humana, Inc. affiliate that provides primary-care, pharmacy, and home health services—when he called the phone number on the back of his Humana Medicare Advantage insurance card to get help finding a doctor.
At his first appointment, Moore recalls, his doctor spent almost an hour with him, not just addressing his respiratory issues that necessitated antibiotics but also getting to know him on a deeper level. This type of quality time with a patient is a hallmark of CenterWell’s focus on value-based care—a patient-centered, outcome-based model of care that aims to lower costs and help patients get healthier. It also allows the doctor to create a personalized care team for each patient, often with a community health worker, a behavioral health specialist, and a pharmacist all working together. Moore recalls leaving his appointment with a much stronger sense of support as a patient compared to previous experiences with the health-care system.
“I haven’t had many doctors in my lifetime that actually sat there and listened to me,” Moore says. “But at CenterWell, the doctors and the nurses don’t rush you in and out. They spend time with you.”
After the doctor addressed Moore’s most pressing health issues, a pharmacist on his care team at CenterWell helped him consolidate and lower his prescription costs. Maegan Burns, the community health worker on his CenterWell care team, helped him find temporary housing, secure transportation to and from his medical appointments, and connect with a local agency that provides food for pets. She continues to be a regular resource for Moore, helping him navigate his insurance and disability benefits when he has questions or concerns.
“I want people to know that they should never feel ashamed to ask for help,” Burns says. “A lot of our older patients are transient. They don’t have family members here. So, helping them find transportation or connect to food services, or calling the insurance company with them to explain how their benefits work—those things can mean a lot to people.”
Understanding what older adults need
People are living longer than ever before, with forecasts showing that 1 in 6 people will be 60 or older by 2030. The vast majority will face at least one chronic condition that requires medical support. National health spending is already more than $4 trillion, and yet an estimated 112 million American adults are struggling to pay for health care. More than double that number say they feel that what they do pay is not worth the cost.
“Historically, I think we’ve done a pretty terrible job in this country of taking care of our elders,” says Kate Goodrich, M.D., Humana’s chief medical officer. “It’s time to do better.”
As the primary caregiver for her own mother, an 86-year-old Medicare Advantage plan member, Dr. Goodrich understands the challenges older adults face firsthand. “Seniors are dealing with so many issues that are specific to their stage of life—from memory loss to cognitive decline to loneliness and isolation and other areas of mental anguish,” she says. “Those things all require the attention of a good primary-care doctor. It’s not just about medical issues. It’s about holistically understanding a patient’s well-being and helping them live a healthy life.”

Health-care insurers, particularly those in the Medicare Advantage system, play a critical role in providing care for seniors. But now they have an even bigger responsibility and opportunity to better serve older adults from diverse backgrounds and make a real impact on patients’ quality of life. One of the ways Humana does that is by offering affordable, accessible, data-driven, and coordinated care through its senior-focused primary-care organization that includes CenterWell Senior Primary Care, which operates primary-care facilities designed specifically for seniors, like the one where Moore is a patient. Humana also encourages and develops value-based care relationships with other providers beyond CenterWell, providing innovative tools that include centralized reporting platforms and actionable data, which in turn creates a better network of interdisciplinary care for the patient.
“It’s important to offer seniors an experience that is just leaps and bounds better than what they’ve had before,” says Dr. Goodrich. “The value-based care model we’re using is designed to meet the holistic needs of seniors because it incentivizes clinicians to spend more time with their patients, which is really what most doctors want to do. That’s the part of our work that allows for the most professional joy.”
Getting to the heart of value-based care
The goal of value-based care is to align financial incentives for providers with four key benefits for patients: increasing prevention and quality of care, measuring outcomes and health-care usage, improving the patient-physician experience, and lowering health-care costs and patient out-of-pocket payments. In other words, providers in this system get paid primarily for delivering better outcomes for patients, not for seeing a higher volume of them or for ordering a higher number of tests.
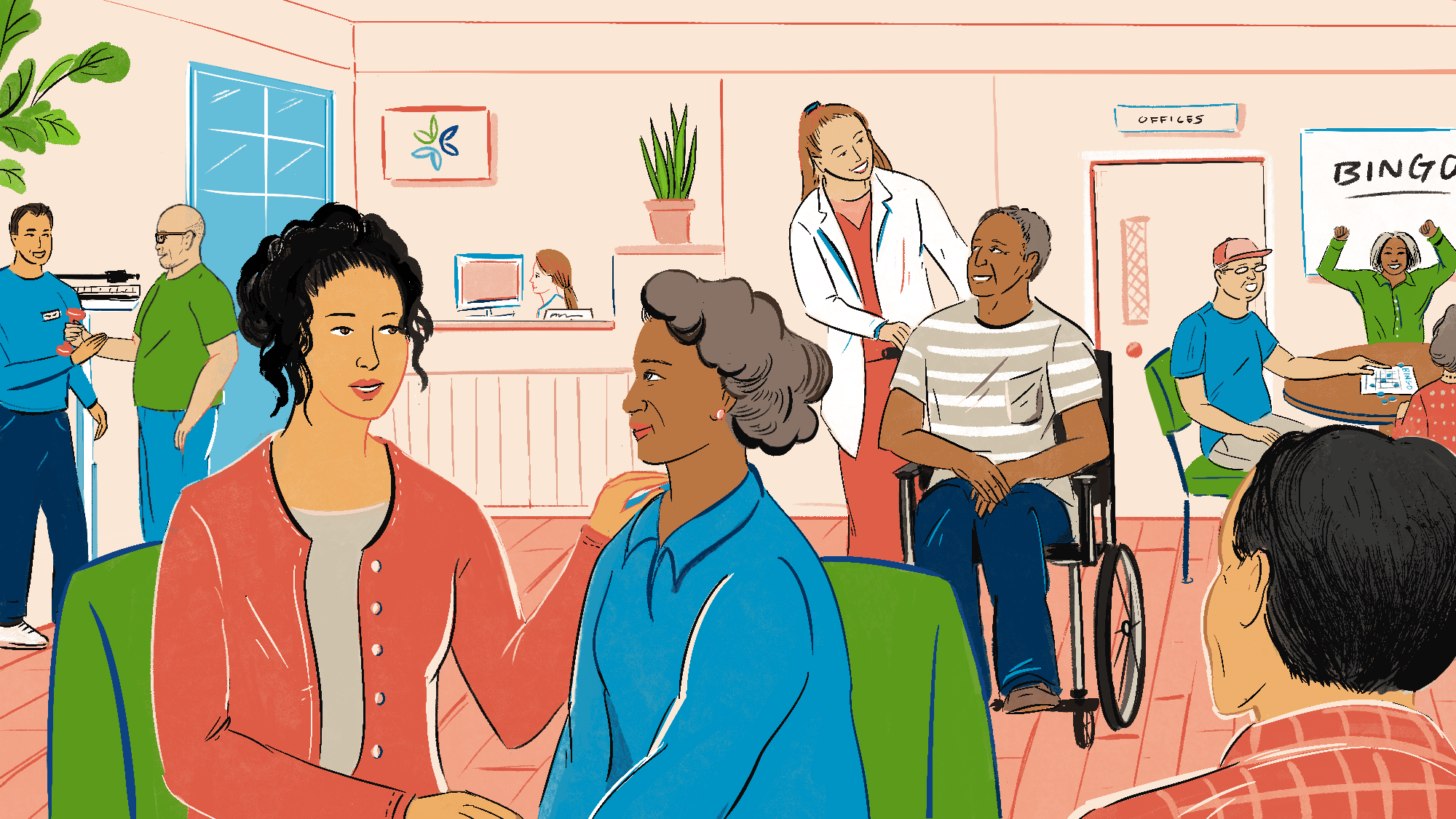
Through value-based care models like those at CenterWell, the path to support is clear: patients have a reliable point of contact, and they are encouraged to call their doctor’s office before going to the hospital. When they arrive, they experience shorter wait times and longer appointments with a doctor. They have easy access to an online portal to view their medical history. They receive compassionate, attentive care that includes preventive screenings, behavioral health services, and online health education classes. Many centers even offer group activities and other community resources for seniors. The facilities are designed to be accessible, with wider hallways for people using wheelchairs and walkers. And they are staffed by a tech-empowered team of people, including community health workers like Burns who contribute to improving care experiences and outcomes while maintaining cost-effectiveness.

The results so far are noteworthy: According to Humana’s most recent “Value-Based Care Report,” in 2022, members with value based care providers saw their primary-care physicians 10 percent more than patients with providers in non-value based care arrangements. In addition, patients with Medicare Advantage plans with physicians in value-based care arrangements saw 30.1 percent fewer in-patient admissions in 2022 versus those enrolled in traditional Medicare. Lastly, Medicare Advantage members who saw value-based care providers reported 12.7 percent fewer emergency room visits in 2022 than those with Medicare Advantage plans that saw non-value based care providers.
While Moore still struggles to afford the rising cost of rent in Las Vegas, he does have temporary housing, and he’s secured part-time work as an usher in guest services at local concerts and sports events, even working the Super Bowl this year. He continues to be a patient at CenterWell.
“They’ve just gone above and beyond for me,” Moore says. “I’m grateful to everybody at CenterWell who knows me and cares about me.”