Two and a half weeks ago, as the next school year approached, a pediatric cardiologist from Louisiana headed into the Georgia mountains with her husband, their three young children, and their extended family. It was, in many ways, a fairly pandemic-sanctioned vacation: All nine adults in attendance were fully vaccinated. The group spent most of the trip outdoors, biking, swimming, and hiking.
Then, on the last night of the outing—July 27, the same day the CDC pivoted back to asking vaccinated people to mask up indoors—one parent started feeling sick. A test soon confirmed a mild breakthrough case of COVID-19. None of the other adults caught the coronavirus on the trip, the cardiologist told me, which she points to as “total proof that the vaccine worked.” (The Atlantic agreed not to name the cardiologist to protect her family’s privacy.) But within a week, six of the eight kids on the trip—all of them too young to be eligible for vaccines—had newly diagnosed coronavirus infections as well.
The infected group included two of the cardiologist’s three sons. Both boys, ages 5 and 11, had just a smattering of cold-like symptoms, the cardiologist said. Even so, the entire ordeal has been rough on their household, which is now split—quite literally—into isolation zones. “My middle son is negative,” she said. “So we have to keep our children on separate floors of our house.” The 7-year-old is missing the first few days of second grade to quarantine. The eldest son, an ardent soccer player about to start sixth grade, had a spate of chest pain and now needs cardiac clearance before he’s able to take the field again.
The family’s predicament is a microcosm of the dangerous and uncertain moment so many Americans face as the pandemic once again changes course. The COVID-19 vaccines have done an extraordinary job of stamping out disease and death. But as the hypertransmissible Delta variant hammers the United States, the greatest hardships are being taken on by the unvaccinated, a population that includes some 50 million children younger than age 12. Across the country, pediatric cases of COVID-19 are skyrocketing alongside cases among unimmunized adults; child hospitalizations have now reached an all-time pandemic high. In the last week of July, nearly 72,000 new coronavirus cases were reported in kids—almost a fifth of all total known infections in the U.S., and a rough doubling of the previous week’s stats. “It’s the biggest jump in the pandemic so far” among children, Lee Beers, the president of the American Academy of Pediatrics, told me. Last week, that same statistic climbed to nearly 94,000.
The most serious pediatric cases are among the pandemic’s worst to date. In the South, where communities have struggled to get shots into arms and enthusiasm for masks has been spotty, intensive-care units in children’s hospitals are filling to capacity. In several states, health workers say that kids—many of them previously completely healthy—are coming in sicker and deteriorating faster than ever before, with no obvious end in sight.
Kids remain, as they have been throughout the pandemic, at much lower risk of getting seriously sick with the coronavirus, especially compared with unvaccinated adults. But the recent rash of illnesses among the nation’s youngest is a sobering reminder of the COVID-19 adage that lower risk is not no risk. With so many children unable to access vaccines and their health contingent on those around them, parents and guardians must now navigate the reality that Delta represents a more serious danger to everyone—which means it’s a more serious danger to kids as well.
One of the worst parts of Delta’s summer upswing, health workers told me, is that so many of them felt powerless to stop it. The United States got a grim preview of the variant’s substantial powers when it first pummeled other countries—India, the United Kingdom—in several spots, battering unvaccinated adults before seeping down to kids. By the time Delta was spreading in earnest in America, many residents had declared the pandemic more or less over, loosening restrictions, reopening businesses, and shedding their face coverings. “As soon as mask mandates went away, COVID came back,” Angela Brown, a charge nurse at St. Louis Children’s Hospital, in Missouri, told me. “And it’s back more than it was last year.” All the while, Delta was establishing itself as a more formidable foe than the ones that had come before it—more contagious, more antibody-evasive, and, according to some early and tentative data, more apt to drive disease.
Vaccines can still tame variants, but only half of Americans have gotten all the shots they need for protection against COVID-19. And those jabs have been doled out unequally, concentrating in certain age groups, geographical regions, and communities privileged by wealth, race, and educational attainment. Kids younger than 12 still aren’t eligible for shots and might need to wait until fall or winter for their green light to come through; teens, who got the FDA’s emergency nod in May, have so far been inoculated at a disappointingly low rate, far below the national average. The situation is especially bad, experts told me, in places where children can’t be cocooned by their communities—areas where rates of vaccination and adherence to infection-prevention measures have lagged in lockstep.
The timing of Delta’s pediatric spike couldn’t have been worse. Many hospitals have for months been cracking under pressure from an unseasonal surge of respiratory syncytial virus (RSV) and parainfluenza—two other airway pathogens that can cause serious illnesses in the very young. Both viruses, typically fixtures of the chilly late-autumn and winter months, had all but evaporated during their typical November-to-February heyday, likely suppressed by pandemic-caliber masking and distancing. When those precautions began to slip, “boom, RSV hit us like a boulder,” Sharon Stoolman, a pediatric hospitalist at Children's Hospital & Medical Center in Nebraska, told me.
The usual influx of pediatric traumas and the unresolved strain on hospitals from the pandemic’s relentless 18-month slog add to the stress. Several health workers told me they were terrified that they’d be unable to provide adequate care to all the sick children coming their way. “My hospital is full today—I don’t have a bed,” Melissa J. Sacco, a pediatric critical-care physician at UVA Children’s Hospital, in Virginia, told me last week. “And I’m just thinking, Please, nobody get run over by a lawn mower.”
“It’s been surreal this past month,” Evelyn Obregon, a pediatric resident at the University of Florida Shands Children’s Hospital, told me. “I’ve never seen this many COVID-positive cases.” Her state is consistently reporting among the highest numbers of pediatric coronavirus cases in the country. Obregon has grown accustomed to treating about five kids with COVID-19 a night; last year, a more usual number was one. In mid-July, she treated a 2-year-old gripped with fever and dehydration. “I was shocked,” she told me. “I had never seen a toddler getting infected like this before.” Her patients are only getting younger, sometimes just weeks old. Most of her patients, she said, are from unvaccinated families.
In recent weeks, Arkansas Children’s—the only pediatric hospital system in Arkansas, where vaccine uptake has been especially sluggish—has admitted far more children than at any other point in the pandemic, Jessica Snowden, the hospital’s chief of pediatric infectious disease, told me. “All of them are unvaccinated.” Last year, she said, she and her colleagues considered it a bad day when they had five to seven kids with COVID-19 in their hospital. Now they’re routinely caring for 20 or 30, nearly half of whom are under 12.
Many of Arkansas Children’s new COVID-19 patients are also much more ill than before. They’re coming in with wrecked lungs, struggling to breathe; they’re not bouncing back with typical youthful resilience, despite having been very healthy before. “This COVID surge, I’ve never seen anything like it,” Linda Young, a respiratory therapist who’s been on the job for 37 years, told me. “It’s the sickest I’ve ever seen children.” It’s become common for more than half of the kids in the ICU to be on ventilators. A few have been in the hospital for more than a month. “We are not able to discharge them as fast as they are coming,” Abdallah Dalabih, a pediatric critical-care physician, told me. Some parents, Snowden said, are in disbelief. “Many people didn’t believe kids could get this thing,” she said.
These early manifestations of disease will likely be just the beginning. One of the most devastating consequences of a pediatric coronavirus infection is a rare complication called MIS-C—an inflammatory condition that burbles up several weeks after a kid first encounters the virus. Some 4,000 cases of the condition have been logged throughout the course of the pandemic so far, many of which have led to full recoveries. But with Delta’s current trajectory, the country might be on the cusp of a glut of new diagnoses. “For me, that’s what I’m more scared of—what things will look like in a month,” Amelia Bray-Aschenbrenner, a pediatric emergency-medicine fellow at St. Louis Children’s, told me. Also looming is the possibility of long COVID, which can saddle people of all ages with weeks of fatigue, brain fog, and joint pain.
What’s happening in the South might be a preview for the rest of the country. In Nebraska, “we are just starting to see the trickle,” Stoolman told me. The adult wards are now full and running low on staff and equipment. That means the pediatric population is next: “This week,” she told me, “we are holding our breath.”
Amid all the chaos is perhaps one tentative silver lining for children. The new variant appears to be following the long-standing trend that kids are, on average, more resistant to the coronavirus’s effects. Although Delta is a more cantankerous version of the virus than its predecessors, researchers don’t yet have evidence that it is specifically worse for children, who are still getting seriously sick only a small fraction of the time. Less than 2 percent of known pediatric COVID-19 cases, for instance, result in hospitalization, sometimes far less.
The alarming rise of pediatric cases seems to reflect the grimness of infectious arithmetic: More kids are falling ill because more children are being infected; more children are being infected because this virus has seeped so thoroughly into the communities most vulnerable to it. America’s pandemic portrait has, after all, warped since the early spring. People of all ages have been venturing back into social settings, often without masks. Kids are no longer being cloistered as vigilantly at home. “The more transmission you have, the more cases you have, and the more you’re going to get bad outcomes,” Sallie Permar, the chair of pediatrics at NewYork-Presbyterian Komansky Children’s Hospital, told me.
Reports of more sickness—maybe even distinct sickness—from states such as Arkansas are worrisome. But maybe these startling effects are explicable. Permar said she isn’t yet seeing this trend play out on a national scale, particularly in states where demand for vaccines has been high. Perhaps kids in high-transmission states, where exposures to Delta are heavy and frequent, are simply being hit with more virus. Delta is already ace at accumulating in the airways of people of all ages, more frequently and more consistently than any variant before, according to Jennifer Dien Bard, the director of the clinical microbiology and virology laboratory at Children’s Hospital Los Angeles. More inbound pathogen might further increase the amount of virus that sticks around to run roughshod over the body. That said, experts told me, it’s still possible that new data could pinpoint a unique effect of Delta on children, especially because so much of what we know already comes from studying adults.
The United Kingdom offers some encouraging clues, and might serve as a bellwether for America’s coming months. The variant’s recent reign triggered a climb in pediatric cases there as well, but kids didn’t seem to make up an unexpected proportion of the surge, Alasdair Munro, a pediatric infectious-disease physician at the NIHR Southampton Clinical Research Facility, told me. As things stand, he said, “there’s no indication” that Delta poses a particular menace to kids.
Kids’ bodies can and do fight back, though an explanation for their tenacity remains elusive. One idea posits that kids’ airway cells might be tougher for the coronavirus to break into, Stephanie Langel, an immunologist at Duke University, told me. Another proposes that their immune system is especially adept at churning out an alarm molecule that buttresses the body against infection. Kids, Langel said, might even have a way of marshaling certain antibodies faster than adults, stamping out the virus before it has a chance to infiltrate other tissues.
Another upside is that although the coronavirus may be changing, the tools that thwart it haven’t. Delta is a substantial enemy, but not an undefeatable one. To protect kids, the AAP has championed the same layered approach that protects adults: combining masks, good ventilation, hygiene, physical distancing, access to testing, and vaccines for everyone who’s eligible. This tag-team tactic will be especially important as kids head back to school in droves this month and next, Grace Lee, a pediatrician at Stanford University, told me.
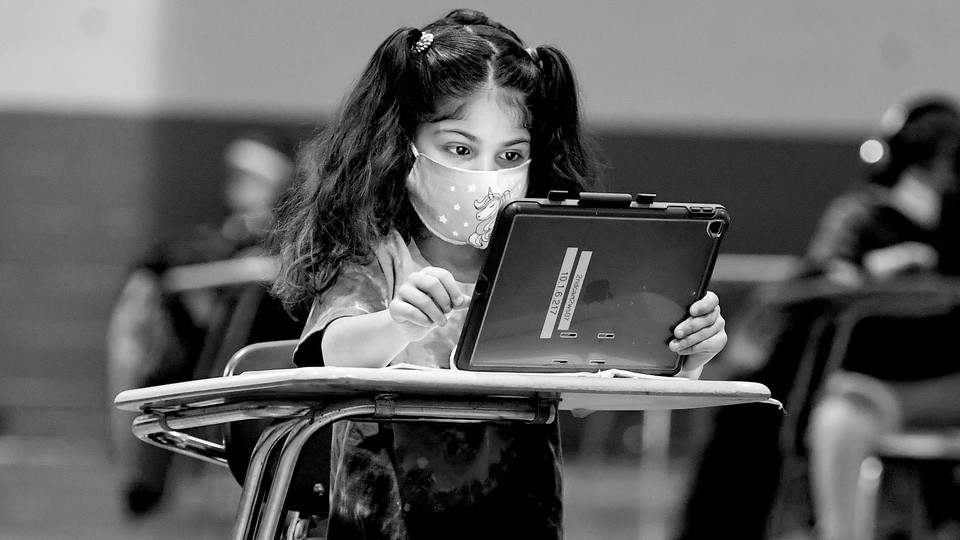
Of course, masks are particularly contentious. Not all countries agree on the best approach when it comes to kids. The World Health Organization doesn’t recommend face coverings for children younger than 6. In the U.K., children under 11 haven’t routinely masked during the pandemic, and Munro says that, apart from strict quarantine and isolation protocols, schools in the U.K. will be looking “more or less normal” this year. In the U.S., though, where vaccine uptake has been a disastrous patchwork and the health-care system has already come under off-season strain, the CDC has recommended universal masking in schools for everyone older than 2. Every expert I spoke with stood behind the guidance: Face coverings and other safeguards, they said, would be a must for a successful academic year. Months of data have reinforced the notion that schools haven’t been a significant source of spread for the coronavirus, Beers, the AAP president, told me, which has led the organization to to strongly recommend that children return to in-person learning. But that evidence was amassed, she stressed, “with careful precautions in place,” including masking.
The fates of young Americans are already splintering—and figuring out what’s best for them has, yet again, been punted to states, counties, districts, and individual families. This creates a particularly thorny decision matrix for parents. Sacco, the pediatric critical-care physician in Virginia, said she’s relieved her first grader and third grader will be attending school with a mask mandate in place. But governors in some states, including Florida and Texas, have spoken out vehemently against school masking mandates. Many districts have already announced plans to go mask-optional.
Ariangela Kozik, a microbiologist in Michigan, told me she’s anxious about sending her 5-year-old son, Alex, into a classroom where he might be one of the only children with a covering on his face. Her district has yet to issue clear masking guidelines. Alex was supposed to enter kindergarten last year, but Kozik and her partner decided to delay his start out of concern for his safety. They’re eager to move forward, and Alex will be wearing a mask no matter what, Kozik said. “I’m crossing my fingers that everyone else will be too.”